Where Medicine Actually Happens
Medicine isn’t practiced at a desktop. It happens in exam rooms between patient conversations. On hospital wards during morning rounds. In the middle of the night when a resident needs an answer and needs it now.
Yet for years, clinical decision support tools have anchored physicians to computers—forcing them to interrupt patient care, retreat to a workstation, search through multiple systems, and piece together fragmented information. The clinical AI market is projected to reach $40.56 billion by 2031, driven by demand for tools that actually fit into clinical workflows rather than disrupting them.
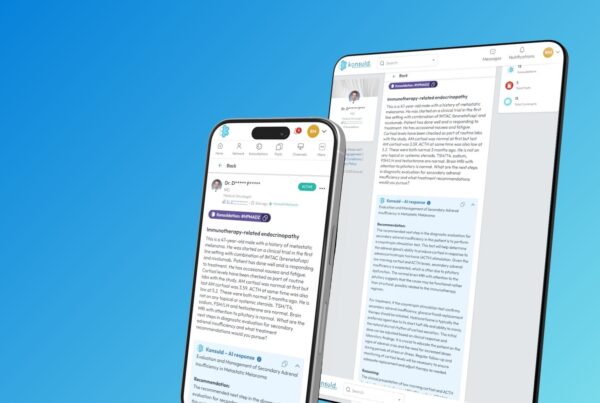
That’s why Konsuld® built native iOS and Android apps designed for one simple purpose: delivering clinical intelligence exactly where and when physicians need it—at the point of care.
The Point-of-Care Problem: Desktop Medicine in a Mobile World
The transition to “desktop medicine” created an unexpected crisis. Physicians now spend up to 60% of their time on non-patient-facing tasks, primarily managing electronic health records and administrative burden. Primary care providers face an impossible mathematical reality: they would need nearly 27 hours daily to meet all nationally established guidelines for patient care while managing EHR workload.
The result? Physician burnout rates reached 63% during the pandemic and remain elevated at 48% in 2023, with administrative burden—not patient care—driving the majority of stress. EMR use correlates directly with burnout, and inefficient clinical tools compound the problem rather than solving it.
Traditional clinical decision support systems, while valuable, often add to this burden. They require physicians to:
- Navigate away from the patient
- Open multiple applications
- Manually search through databases
- Toggle between reference materials and clinical documentation
- Synthesize information across disconnected systems
Each context switch costs time and mental energy, resources physicians can’t afford to waste when patient care hangs in the balance.
The Knowledge Graph Advantage: Structure Beneath the Surface
Konsuld’s mobile apps solve this problem through architecture, not just interface design. At the foundation sits a clinical knowledge graph—a structured map of medical knowledge that connects physicians, conditions, therapies, clinical trials, and treatment guidelines into a living, queryable network.
Recent research in Annual Reviews of Biomedical Data Science demonstrates that knowledge graphs enhance interpretability by aligning AI-driven insights with established medical knowledge. Unlike generic large language models that may hallucinate or provide inconsistent responses, knowledge graph-constrained systems deliver responses grounded in traceable, domain-specific evidence.
Here’s how Konsuld’s knowledge graph works in practice:
Nodes represent clinical entities: diseases, treatments, physicians by specialty, clinical trials, practice guidelines, drug interactions, patient populations, and more.
Edges represent relationships: “treats,” “contraindicates,” “approved for,” “commonly prescribed in,” “evidence from,” and dozens of other semantic connections that mirror how expert clinicians actually reason.
Graph traversal enables reasoning: When a physician asks about second-line therapy for a specific patient population, the system doesn’t just keyword-match. It traverses the graph: starting from the condition → following edges to treatments → filtering by patient characteristics → checking contraindications → prioritizing based on current guidelines and specialty-specific practice patterns.
Constraints prevent hallucination: The AI can only “see” and reason over graph-validated, specialty-aligned content. If a relationship doesn’t exist in the knowledge graph, the AI cannot invent it. This architectural constraint dramatically reduces the risk of clinical misinformation.
A 2024 study in JMIR AI showed that knowledge graph systems outperformed standard LLMs in diagnostic reasoning by providing contextually relevant paths aligned with medical ontologies like SNOMED CT. The structured approach reduced errors while increasing explainability—both critical for clinical adoption.
Voice-First Clinical Intelligence: Asking Questions Naturally
The Konsuld mobile experience begins with voice. A physician can speak a clinical question using voice-to-text without typing, navigating menus, or reformulating queries to match database search syntax.
Consider a complex oncology question: “Second-line options for a frail 78-year-old with metastatic ER+/HER2– breast cancer after CDK4/6 progression?”
This single spoken question contains multiple clinical nuances:
- Patient age and frailty status (affecting treatment tolerance)
- Specific cancer subtype (ER+/HER2–)
- Disease stage (metastatic)
- Prior treatment line (CDK4/6 inhibitor)
- Clinical scenario (progression, requiring next therapy)
Konsuld’s system:
- Transcribes the spoken query accurately using medical terminology recognition
- Structures the question by identifying key entities (patient characteristics, disease, prior treatment, clinical need)
- Routes the query through the knowledge graph, traversing nodes for metastatic breast cancer → treatment options → filtered by ER+/HER2– → second-line therapies → adjusted for elderly/frail populations → validated against current NCCN guidelines
- Generates a targeted response with clear rationale and evidence citations
The entire process takes seconds. The physician never leaves the patient’s bedside. The answer arrives grounded in current evidence, specialty-specific guidelines, and real-world treatment patterns.
The Clinical Workflow Integration: Fast Enough to Matter
Speed matters in clinical decision support. Research shows that point-of-care clinical decision support can reduce physician workload by up to 36% when designed for actual workflows rather than theoretical use cases.
Konsuld’s mobile apps prioritize three workflow principles:
Minimal friction to answer: Open app → speak question → receive answer. No account switching. No multi-step navigation. No reformulating queries.
Between-patient timing: Designed for the 2-5 minute gaps between seeing patients. Physicians can quickly verify a dosing question, check for drug interactions, or review treatment guidelines without delaying patient flow.
Specialty-aligned by default: The system knows the user’s specialty and adjusts recommendations accordingly. An internist and an oncologist asking about the same condition receive answers tailored to their respective scopes of practice.
The clinical decision support market is increasingly recognizing that mobile-based platforms will drive adoption, with healthcare organizations prioritizing tools that physicians actually use over comprehensive systems they theoretically could use.
Rigorous Enough for Specialists: Depth Without Compromise
Mobile doesn’t mean simplified. Konsuld maintains clinical rigor through:
Evidence-based content: Only peer-reviewed medical literature, clinical practice guidelines, and FDA-approved drug information enter the knowledge graph. No social media. No patient forums. No unvetted sources.
Specialty-specific reasoning: The knowledge graph includes specialty-specific treatment patterns, preferred regimens, and nuanced considerations that general medical resources often miss.
Transparent citations: Every recommendation includes clear references to supporting evidence. Physicians can trace the reasoning chain and verify sources directly.
Continuous validation: The system undergoes ongoing quality assurance through automated regression testing and clinical expert review to detect drift or outdated recommendations as medical knowledge evolves.
Real-World Impact: What Changes at the Bedside
When clinical intelligence becomes genuinely mobile and frictionless, practice patterns shift:
Fewer delayed decisions: Instead of noting “check X and follow up tomorrow,” physicians can get immediate answers and make real-time adjustments to care plans.
Reduced cognitive load: The system handles information retrieval and synthesis, freeing mental capacity for higher-order clinical reasoning and patient interaction.
Better patient conversations: With instant access to current evidence, physicians can have more informed discussions with patients about treatment options, risks, and alternatives.
Specialty consultation without delays: For complex cases requiring specialty expertise, the AI provides specialty-aligned guidance that may prevent unnecessary formal consultations or help prepare more focused questions for specialists.
Healthcare organizations implementing well-designed point-of-care clinical decision support report significant improvements in clinician satisfaction when tools genuinely reduce administrative burden rather than adding to it.
The Architecture of Trust: Why Structure Matters for Safety
Clinical AI carries inherent risks. Generic large language models have been shown to hallucinate drug dosages, contraindications, and treatment recommendations. A 2024 Nature Medicine commentary emphasized that continuous validation and monitoring are as critical as initial accuracy for patient safety.
Konsuld’s knowledge graph architecture provides multiple layers of safety:
Bounded reasoning space: The AI can only traverse validated relationships in the knowledge graph. It cannot invent connections that don’t exist in verified medical knowledge.
Traceable inference chains: Every recommendation can be decomposed into the specific graph paths that led to it, making the reasoning process auditable and verifiable.
Specialty constraints: The system prevents recommendations outside a physician’s scope of practice or specialty expertise.
Continuous monitoring: Automated quality checks detect when recommendations drift from validated patterns, triggering human expert review.
Patient-centric knowledge graphs, as detailed in recent Frontiers in Artificial Intelligence research, enable more personalized and effective care while maintaining interpretability—essential for clinical decision-making where explainability directly impacts physician trust and adoption.
Market Context: The $3.89 Billion Clinical Decision Support Opportunity
The clinical decision support market is experiencing rapid growth, projected to reach $3.89 billion by 2030 at a 9.6% CAGR. Key drivers include:
- Rising adoption of healthcare IT solutions
- Increasing demand for better clinical outcomes
- Growing concerns over medication errors and patient safety
- Advancements in AI, machine learning, and natural language processing
- Government initiatives promoting digital health infrastructure
By 2024, 66% of U.S. physicians reported using AI in their practice, up from just 38% in 2023, with clinical decision-making support emerging as a primary use case.
For healthcare innovation, the opportunity lies in solutions that demonstrate:
- Measurable clinical outcomes: Improved diagnostic accuracy, reduced medication errors, enhanced treatment adherence
- Physician adoption metrics: Daily active usage, time savings, satisfaction scores
- Workflow integration: Seamless incorporation into existing clinical patterns
- Scalability: Ability to expand across specialties and care settings
Konsuld’s mobile-first, knowledge graph-based approach positions it within this high-growth segment while addressing the core physician pain points driving burnout and workflow inefficiency.
For CMIOs and Health System Leaders: Implementation Considerations
Chief Medical Information Officers evaluating mobile clinical decision support should consider:
Integration requirements: Does the solution require extensive EHR integration, or can it function independently while still providing value?
Specialty coverage: Can the system serve the breadth of specialties in your organization, or is it limited to primary care or specific domains?
Evidence standards: What sources inform the system’s recommendations? Are they independently verifiable and consistent with institutional guidelines?
Update mechanisms: How does the system incorporate new medical evidence and guidelines? What’s the lag time between publication and implementation?
Usage analytics: Can you track adoption patterns, query types, and clinical outcomes to demonstrate ROI?
Governance framework: What oversight mechanisms ensure ongoing quality and safety as the system evolves?
The most successful clinical AI implementations, according to recent healthcare IT research, combine robust automated monitoring with clinical expert review and physician feedback integration—exactly the approach Konsuld employs for lifecycle management.
The Path Forward: Clinical Intelligence Everywhere Medicine Happens
The future of clinical decision support isn’t replacing physicians with AI. It’s ensuring that physicians have instant access to comprehensive, current, evidence-based medical knowledge wherever they practice medicine.
Konsuld’s mobile apps represent a step toward that future:
- Clinical questions answered in seconds, not minutes
- Evidence-based recommendations grounded in knowledge graphs, not generic models
- Specialty-specific guidance that respects the depth and nuance of expert practice
- Truly mobile intelligence that follows physicians throughout their day
As one physician noted in burnout research: “I spend more time looking at a computer than seeing patients.” Mobile clinical AI offers a counterbalance—bringing computational support to patient care rather than pulling physicians away from it.
The technology is ready. The need is urgent. Medicine happens at the bedside, and clinical intelligence should too.
Download Konsuld® today:
- iOS: App Store
- Android: Google Play

Chief Artificial Intelligence Officer – Konsuld
I am an entrepreneurial data architect with a record of successes. I am creative, analytical and a curious problem solver who defines and drives strategic and tactical growth. Record of taking products from initial product conception to customer installation. A thought leader who puts thought into practice. Konsuld is a clinician-exclusive platform revolutionizing patient care through seamless collaboration and cutting-edge AI-driven tools. We integrate diverse medical data sources, like PubMed and medical guidelines, to provide HCPs with actionable insights in real-time.